Research and Articles
Effects of Pressurized Oxygen in Acute Brain Insult
Effects of Pressurized Oxygen in Acute Brain Insult
hyperbaricstudies.com/research-studies/effects-of-pressurized-oxygen-in-acute-brain-insult/
September 25, 2013
From the 3rd International Symposium for Cerebral Palsy and Brain-Injured Child
- Reduces cerebral edema & ICP
- Limits the ischemic cascade
- Reduces CNS lactate peak in hypoxia
- Neutralizes toxic amines
- Deaggragation of platelets
- Increases Phagocytic activity of PMN cells (white blood cells)
- Reduces Adhesiveness of WBCs to endothelium
- Perfuses all tissues spaces
- Life sustaining O2 available via retrograde perfusion in absence of a trickle phenomena
- Delivers metabolically available O2 without chemical energy transfer – Enough to sustain life without blood
- Under pressure O2 adheres to all the gas laws of physics
- Displaces all other gases in the body: N2, CO
- Follows the Law of Mass Action
- Completely saturates hemoglobin
- Increases plasma O2 by 2000%
- Dissolves in cerebrospinal fluid, lymph, bone, and urine
Effects of Pressurized Oxygen in Chronic Brain Insult
- Reactivates idling neurons
- Enhances plasticity
- Efficiently elevates diffusional driving force for O2 thereby increasing tissue oxygen availability
- Promotes phagocytosis (internal debridement)
- Ameliorates multiple biochemical changes
- Restores the integrity of the blood brain barrier and cell membranes
- Improves cell respiration, Reduces cell byproducts – cytokines
- Promotes Neovascularization
- Promotes Epithelization
- Acts as scavenger of free radicals
- Bacteriostatic effects, synergizes with certain antibiotics
- Neutralizes certain Toxins: Clostridium, anaerobes
- Stimulates the adaptive immune system, especially in elderly (mice)
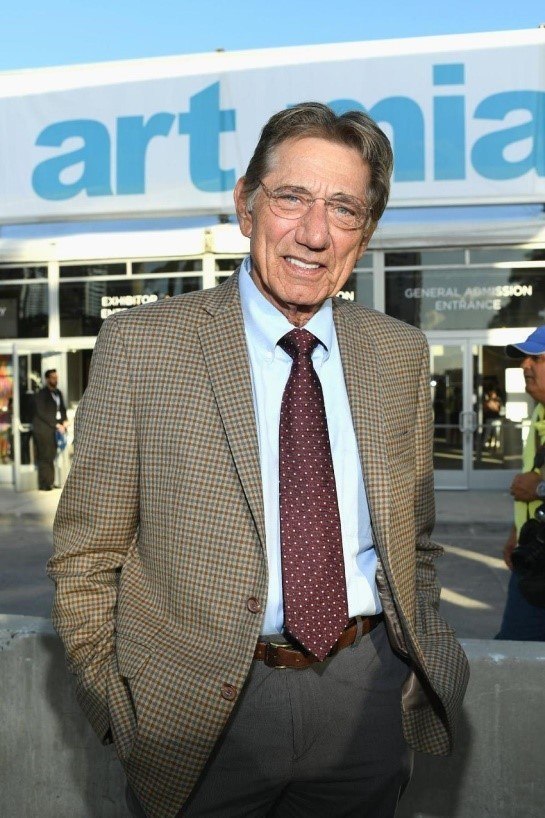
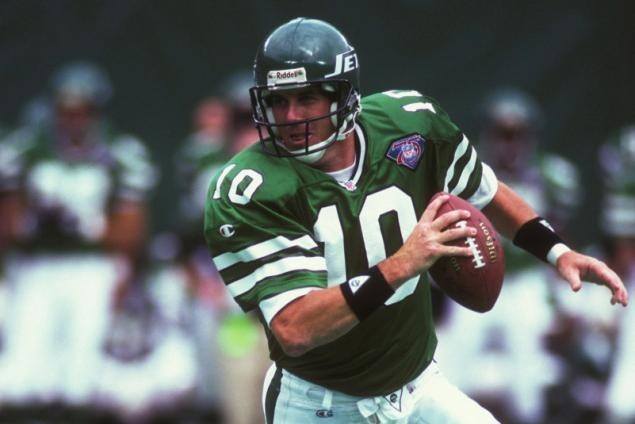
Jets legend Joe Namath has been undergoing hyperbaric oxygen treatments
Broadway Joe is still making waves.
Jets legend Joe Namath told friends that the 120 hyperbaric oxygen treatments known as “Dives” that he's undergone in recent years are showing great results.
The former quarterback went on to say that those sessions, which he underwent at the Jupiter Medical Center in Florida, have helped restore blood flow to the left side of his brain that had been slowed by 12 years of blows to the head during a Hall of Fame career.
“My doctors did flips after looking at the results of my last tests which showed fully restored blood flow to my brain,” Namath told pals in south Florida, where he has a home. “I know several players that committed suicide due to concussions they suffered on the field. I’ve taken the results of my tests to the FDA who have asked for another study with a hundred people.”
The former passer suffered through multiple lower leg injuries during his career and had both of his knees surgically replaced after his playing days were over. Friends were glad to hear Namath say he’s successfully dealing with his head injury as well.
Namath announced the good news while preparing to attend the Jan. 15 opening of Nick Korniloff's Palm Beach Modern + Contemporary Art Fair, which will raise money for The Joe Namath Neurological Center. The event will feature works by Picasso, Warhol, Basquiat and Keith Haring from over 50 galleries form around the world.
“I’m going to raise $10 million dollars to get it done,” Namath forecasted. He famously predicted Gang Green would upset the heavily favored Baltimore Colts in Super Bowl III and they did. This isn't the first time Namath has teamed up with Korniloff. In 2015, when Korniloff's stepson Perry Cohen went missing while fishing with another Florida boy off the coast of Miami, joined in the search for the two 14-year-olds, who were never found.
This isn't the first time Namath has teamed up with Korniloff. In 2015, when Korniloff's stepson Perry Cohen went missing while fishing with another Florida boy off the coast of Miami, joined in the search for the two 14-year-olds, who were never found.
Concussion and Hyperbaric Oxygen Therapy (HBOT)
What is a concussion? Can hyperbaric medicine help?
Concussion is a mild traumatic brain injury that causes bruising and swelling to the brain resulting in disruption of brain function.
Symptoms can present as the following and last for weeks, months or years:
- Headaches
- Brain fog
- Trouble concentrating and reading
- Memory loss
- Irritability
- Difficulty sleeping
- Vision issues
After your doctors have ruled out life threatening conditions such as a brain bleed, you should contact Nirvana Hyperbaric Institute: (805)-693-8100 - Solvang, California.
Hyperbaric Oxygen Therapy (HBOT) can repair the damage and alleviate the symptoms in as few as five treatments if treated within the first ten days following the concussion.
People who sustain a brain injury are 3x more likely to sustain a 2nd brain injury and 8x more likely to sustain a 3rd.
That is why it is important to address all concussions immediately with hbot as it can actually repair the physical damage.


Scientists Have Reversed Brain Damage in a 2-Year-Old Girl Who Drowned in a Swimming Pool
She was in the water for 15 minutes
PETER DOCKRILL
19 JUL 2017
Researchers in the US have reported what they believe is a first-of-its-kind reversal of brain damage, after treating a drowned and resuscitated toddler with a combination of oxygen therapies.
The little girl, whose heart didn't beat on her own for 2 hours after drowning, showed deep grey matter injury and cerebral atrophy with grey and white matter loss after the incident, and could no longer speak, walk, or respond to voices – but would uncontrollably squirm around and shake her head.
Amazingly, thanks to a course of oxygen treatments – including hyperbaric oxygen therapy (HBOT) – administered by a team from LSU Health New Orleans and the University of North Dakota, doctors were able to significantly reverse the brain damage experienced by the toddler.
"The startling regrowth of tissue in this case occurred because we were able to intervene early in a growing child, before long-term tissue degeneration," says hyperbaric specialist Paul Harch from the LSU Health New Orleans School of Medicine.
The drowning occurred in February of last year, when two-year-old Eden Carlson slipped through a baby gate while her mother took a shower, then made it past a heavy door, before eventually falling into the family swimming pool.
She was in the water for 15 minutes before being discovered and had experienced cardiac arrest, and while her mother immediately began CPR, Eden wasn't successfully resuscitated for 2 hours, being eventually revived by doctors at Washington Regional Medical Centre in Fayetteville, Arkansas.
After receiving critical care in hospital for 48 days, the little girl was discharged, but due to the extent of her brain injuries and their physical side effects, Harch proposed treatment with oxygen therapies in an attempt to "wake up" Eden's damaged brain.
Hyperbaric oxygen therapy works by administering oxygen to a patient at an ambient pressure higher than atmospheric pressure, through the use of a sealed, pressurised chamber.
By doing this, the amount of oxygen in a patient's blood supply is increased, which can restore normal levels of blood gases and repair damaged tissue.
In this case, Eden wasn't located close enough to a hyperbaric oxygen therapy chamber, so the team began a bridging course of normobaric oxygen treatments – delivered at sea level pressure – at fifty-five days after the drowning.
The treatments, given for 45 minutes twice a day through a nasal cannula, saw Eden recover alertness and reduced her squirming, giving her back increased movement of her arms and hands.
She also regained part of her ability to eat orally, and could speak short sequences – and laugh.
About three weeks later, the researchers moved Eden and family to New Orleans, where she began a round of new treatments in a hyperbaric chamber.
After just 10 sessions, Eden's mother observed that the toddler was back to "near normal, except for gross motor function", and so the little girl began physical therapy in addition to the hyperbaric treatment.
Once 39 hyperbaric sessions were completed, Eden's walking had improved, and her speech level was assessed to be now greater than it was at the time of the drowning. She demonstrated improvements on all neurological abnormality tests, and showed near normal motor function and cognition.
At the conclusion of the treatment, some 162 days after she drowned, MRI scans revealed that Eden still bore a mild residual injury to her brain, but had experienced a near-complete reversal of cortical and white matter atrophy.
The team studying her recovery say that to their knowledge, this kind of reversal is "unreported with any therapy".
And while they don't fully understand the exact breakdown of this amazing revival in Eden's fortunes, it's clear that normobaric and hyperbaric oxygen treatments combined to reduce inflammation and promote brain cell survival.
"Although it's impossible to conclude from this single case if the sequential application of normobaric oxygen then HBOT would be more effective than HBOT alone, in the absence of HBOT therapy, short duration, repetitive normobaric oxygen therapy may be an option until HBOT is available," Harch says.
"Such low-risk medical treatment may have a profound effect on recovery of function in similar patients who are neurologically devastated by drowning."
The findings are reported in Medical Gas Research.
Update: Since this story was first published, other scientists have voiced their concerns about whether the oxygen treatments administered to Eden could explain her recovery as suggested in the study.
In comments made to Live Science, paediatric neurologist Ian Miller from Nicklaus Children's Hospital in Miami cast doubt on whether hyperbaric and normobaric treatments could deliver such a result.
"There is just no way that providing oxygen to a dead brain cell makes the brain cell recover," Miller told Live Science's Rachael Rettner. "That's not how the brain responds to injury and to oxygen once neurological death has occurred."
His concerns were shared by physiotherapist David Cifu from Virginia Commonwealth University, who said Eden's recovery was more likely due to factors other than hyperbaric treatment, which was unlikely to have restored her lost brain functions.
In separate comments, consultant anaesthetist Oliver Sykes from University College London told The Independent that there's no evidence that hyperbaric treatment can produce recoveries like this.
"I can't think of a reason why what has been reported would have happened, and I'd be very surprised if this was a repeatable result," he said. "I haven't heard of this kind of reported outcome before."
For what it's worth, the FDA warns people on its website that hyperbaric treatments have been touted to deliver a range of medical benefits for various ailments, but many of the results aren't clinically proven.
In response to his detractors, Harch told Live Science that Eden made "progressive accelerated neurological improvement with each week of HBOT…. Spontaneous recovery and growth of tissue can possibly occur over time, but the child was not improving at this rate until the introduction of each of these therapies".
As for whether the treatment and recovery in this instance were more than just a coincidence is unclear, but if Harch's claims are correct, hopefully future research into HBOT can clarify what's going on here, and whether we've got a truly viable solution to these kinds of brain injuries.
Until then, we're thrilled Eden has made the recovery she has, but have updated the article with these opinions to give a fuller picture on some of the questions surrounding this area of research.
Management of Haemorrhagic Stroke with Hyperbaric Oxygen Therapy
Case Report
By: J Lim, W K Lim, T T Yeo, Y Y Sitoh, E Low
ABSTRACT
Hyperbaric oxygen therapy (HBOT) has been used in the treatment of cerebral ischaemia with positive effects on tissue oxygenation. We present a case of hemorrhagic stroke treated successfully with HBOT and review the literature on its role in cerebrovascular disease.
INTRODUCTION
Stroke, or “brain attack”, is a leading cause of mortality and morbidity in developed populations. The treatment of thrombo-embolic ischemic stroke has been revolutionized using thrombolytics, but hemorrhagic stroke has no such equivalent and its past management was often gloomy and bereft of any “active” therapy. The primary pathology is that of lack of tissue oxygenation and Illingworth et al in 1961 suggested that HBOT could be beneficial in cerebrovascular disease.
Its use in the treatment of cerebral ischemia was first reported by Ingvar and Lassen four years later.
Of their four patients, three improved and the fourth did show dramatic initial improvement before succumbing to thrombotic lesions in the brainstem.
Since then, more than 1,000 cases have been reported world-wide and since last year, the Naval Medicine and Hyperbaric Centre (NMHC) began treating selected intracerebral hemorrhages with HBOT. We wish to present here a typical case of a patient treated with HBOT.
CASE REPORT
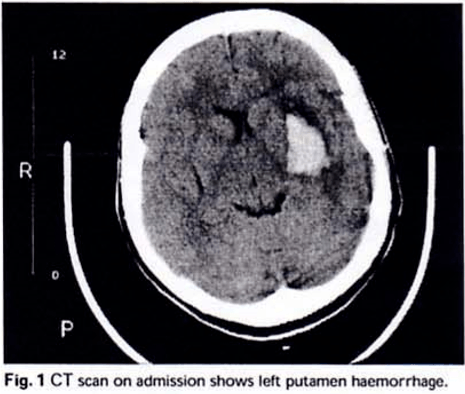
SYL, a 48-year-old Chinese lady with a two-year history of hypertension, presented to a local hospital with right-sided weakness associated with giddiness and slurred speech. Initial examination revealed a slight dulling of consciousness (GCS = 10/15: E4, M5, V1) and right-sided hemiparesis (MRC grade 2/5). Tone was increased on the right with upgoing plantar response and there was also an upper motor neuron VII nerve palsy and absent gag reflex. Blood pressure on admission was 196/98 and was stabilized with nifedipine. Emergency CT scan showed a left putaminal haemorrhage (approx. 2 x 3 cm)
As she was haemodynamically stable and the size of the haemorrhage was less than 40 ml, she was selected for non-surgical intervention and referred to NMHC for a trial of HBOT. After assessment to determine her fitness for HBOT, treatment based on the Long Beach table (100% O2 at a depth of 8 metres for 1 hour and 30 minutes; this table originated from work done at the Long Beach Memorial Medical Centre) was initiated.
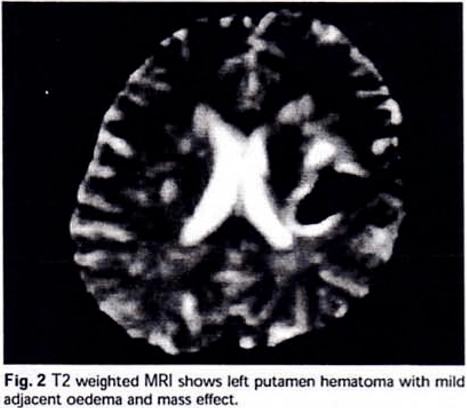
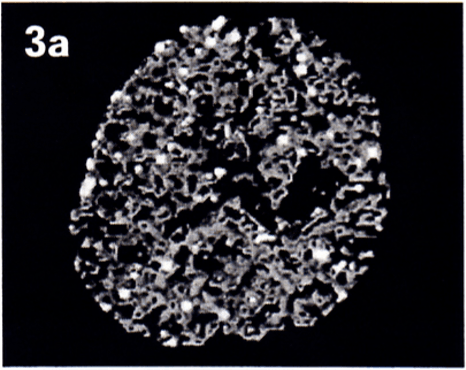
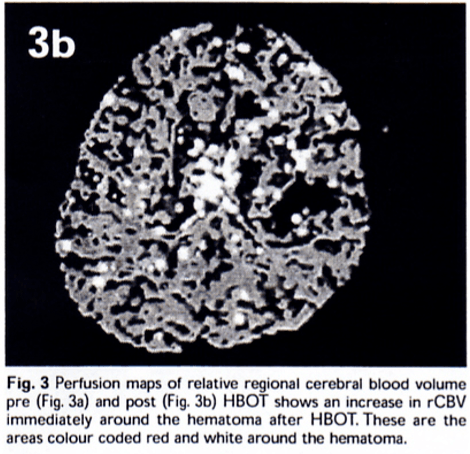
Within 24 hours of onset of symptoms. Dynamic contrast enhanced perfusion weighted functional magnetic resonance imaging (fMRI) was obtained immediately before and after the first session of HBOT treatment. She underwent a total of nine treatments over eight days with no complications of therapy. By the third treatment, her GCS had improved to 15/15. Motor power improved to 4/5 after the fourth treatment but deteriorated to 3+/5 after the fifth treatment. Treatment continued until power improved to 4/5 and we decided to terminate treatment after nine sessions because of a plateau of improvement. There was marked improvement of the facial nerve palsy and the gag reflex had returned. Her improvement was sustained at 3- and at 6-months follow-up.
DISCUSSION
Despite decades of intense debate and research, the optimal management of spontaneous intracerebral haemorrhage is still unresolved. The role of surgery is still controversial for supratentorial haematoma, but a more conservative attitude towards operative intervention has become more acceptable. This is largely due to the generally poor long-term functional outcome regardless of the modality of treatment. Oxygenation is the most critical function of blood flow and in this respect, HBOT has many attractive theoretical benefits. Experimental and clinical data have been encouraging, and with the increasing sophistication of positron emission tomography (PET), single photon emission computed tomography (SPECT) and functional MRI studies including diffusion and perfusion weighted scans, it is probable that the effects of HBOT on cerebral blood flow and metabolism will become better appreciated.
The fMRI techniques have superior spatial and temporal resolution over PET and SPECT; neither do they involve the use of ionizing radiation. In perfusion weighted fMRI, dynamic images are obtained during the first-pass effect of an MRI contrast agent through the brain. Brain perfusion maps of relative regional cerebral blood volume (rCBV) and mean transit time (MTT) of contrast are generated. This semi-quantitative technique can potentially document the changes in perfusion with HBOT treatment.
PROPOSED MECHANISMS OF ACTION
HBOT is essentially the supply of oxygen under pressure to ischaemic areas. The hyperoxic state not only improves oxygenation of ischaemic tissues, but also has beneficial effects of cellular metabolism and intra-cranial pressure.
1. Improvement of oxygenation
HBOT increases the amount of oxygen dissolved in plasma and can nourish tissues even in the absence of red blood cells. Even in total vascular obstruction, plasma has been shown to seep through and deliver oxygen. There is also increased extravascular diffusion because of the greater diffusion gradient and the abundance of capillaries in brain tissue. The supply of oxygen is further facilitated by the induced hyperoxic state decreasing blood viscosity and increasing red cell deformability. Though there is vasoconstriction with reduction in blood flow, this is ameliorated by the alignment of red cells in a column instead of moving randomly (Fahraeus Liindqvist effect). Hence the improved rheology tends to counter the effects of vasoconstriction.
2. Reduction of Intra-Cranial Pressure
Intracranial pressure (ICP) is a function of blood flow, amount of brain tissue and oedema, and the volume of cerebrospinal fluid (Kelly-Munroe doctrine). HBOT, by inducing vasoconstriction, counters the vasodilatation of capillaries in hypoxic tissue and reduces the extravasation of fluid. Blood flow is reduced but tissue oxygenation is not compromised because of the improved delivery of oxygen. However, this effect is short-lived and Kohshi suggests that reduced ICP is maintained during HBO inhalation by induced hypocapnia. With the cessation of a treatment period, normal breathing is resumed and this could account for the initial fluctuation in improvement seen in our patient.
3. Improved metabolic function of cerebral tissue
HBOT has been shown to improve glucose metabolism, and hence prevents glycolysis and intracellular lactic acidosis build-up. Mink and Dutka, working on rabbit models, found that HBOT promoted blood-brain barrier integrity after global cerebral ischaemia, and Japanese studies have demonstrated the HBOT reduces intracellular potassium ion concentration in red cells. The underlying mechanism may relate to restoration of ion pump function in ischaemic cell membranes, and this may prevent the production of potentially damaging vasoactive mediators and facilitate recovery.
THEORETICAL NEGATIVE EFFECTS OF HBOT
There is concern that HBOT may worsen re-oxygenation injury by promoting oxygen free radicals and lipid peroxidation. However, Yasu was only able to demonstrate this in normal rat brains, but not in ischaemic rat brains. Furthermore, rabbit studies from Bethesda, USA, showed that while HBOT increased the number of free radicals, this was not associated with an increase in lipid peroxidation or a reduction in neurophysiologic recovery.
Another criticism of HBOT is that induced vasoconstriction will compromise cerebral blood flow. While HBOT does reduce blood flow, this has not resulted in clinical detriment. It was also not associated with a reduction in evoked potential recovery or cerebral metabolism on SPECT imaging. Hence, we can postulate that cerebral oxygenation is improved with HBOT despite the reduction in blood flow. Another possibility is the inverse steal phenomenon described by Lassen and Palvogyi, in which constriction of vessels in normal brain may increase blood flow in unresponsive areas.
FUTURE DIRECTIONS
HBOT has been described as “a therapy in search of diseases”. Though ischaemic cerebral injury is a theoretically attractive disease to treat with HBOT, it is not one of the indications under the Underseaand Hyperbaric Society guidelines (1992). Nonetheless, the growing body of experimental and clinical experience appears to be favourable. Improvements in functional MRI techniques may obviate the need for large-scale randomized trials (difficult presently because of limited hyperbaric facilities) to demonstrate clinical efficacy as improvement can be documented radiologically and correlated with clinical symptomatology. More work needs to be done on determining the optimum time of administering treatment though, regarding stroke as a “brain attack” will intuitively suggest that the earlier the treatment, the better the outcome. Animal studies combining HBOT with nicardipine administration showed acceleration of neurologic recovery, and combination of HBOT with neuro-protective pharmacological agents and anti-oxidants is likely to further benefit derived.
CONCLUSION
HBOT may be a useful modality in the treatment of spontaneous intracerebral haemorrhage. Evidence thus far has been encouraging, but this has largely been in the form of limited series and case reports and a randomized controlled trial is required to clarify the issue. More work also needs to be done to determine the optimum timing of treatment and to identify patients who would benefit most from HBOT. The role of combining HBOT with pharmacotherapy e.g. anti-oxidants, needs to be explored further. It is envisioned that diffusion and perfusion functional MRI may play a pivotal role in both defining the role of HBOT and elucidating its mechanisms of action.