Main Menu
Contact Us
Jay Kuhn
www.8-Test.com
Jkuhn@MichigandiagnosticTesting.com
South-East Michigan
(248) 524-9905
Autonomic Nervous System (ANS) Testing Treat The Cause - Not the Symptoms
WHAT IS THE AUTONOMIC NERVOUS SYSTEM (ANS)?
The autonomic nervous system (ANS) regulates physiologic processes, such as blood pressure, heart rate, body temperature, digestion, metabolism, fluid, and electrolyte balance, sweating, urination, defecation, sexual response, and other processes. Regulation occurs without conscious control, i.e., autonomously. The ANS has two major divisions: the sympathetic and parasympathetic systems. Many organs are controlled primarily by either the sympathetic or parasympathetic system, although they may receive input from both; occasionally, functions are reciprocal (e.g., sympathetic input increases heart rate; parasympathetic decreases it).
The sympathetic nervous system is catabolic and activates fight‐or‐flight responses. Thus, sympathetic output increases heart rate and contractility, bronchodilation, hepatic glycogenolysis and glucose release, BMR (basal metabolism rate), and muscular strength; it also causes sweaty palms. Less immediately‐life‐preserving functions (e.g., digestion, renal filtration) are decreased.
The parasympathetic nervous system is anabolic; it conserves and restores. Gastrointestinal secretions and motility (Including evacuation) is stimulated, heart rates slowed, and blood pressure decreases.
Disorders of the ANS can affect any system of the body; they can originate in the peripheral or central nervous system and may be primary or secondary to other disorders. Symptoms suggesting autonomic dysfunction include orthostatic hypotension, heat intolerance, nausea, constipation, urinary retention or incontinence, nocturia, impotence, and dry mucous membranes. If a patient has symptoms suggesting autonomic dysfunction, cardiovagal, adrenergic, and sudomotor tests are usually done to help determine severity and distribution of the dysfunction.
Autonomic Regulation is the body’s ability to maintain homeostasis (stability and balance) during internal and external stimuli. Autonomic Regulation is always functioning, and we are often unaware of the important tasks it is performing. When the nerves that control Autonomic Regulation are damaged, Autonomic Dysfunction can develop. Autonomic Dysfunction can be temporary or chronic. Diabetes and Parkinson’s disease are two examples of chronic conditions that can lead to Autonomic Dysfunction.
Cardiovagal innervation testing evaluates heart rate response to deep breathing and to the Valsalva maneuver, via electrocardiogram rhythm strip. If the ANS is intact, heart rate varies with these maneuvers; the ratio of longest to shortest R‐R interval (Valsalva ratio) should be 1.4 or greater.
Vasomotor adrenergic innervation testing evaluates the response of beat‐to‐beat blood pressure to the head‐up tilt and Valsalva maneuver. The head‐up tilt shifts blood to dependent parts, causing reflex responses. The Valsalva maneuver increases intrathoracic pressure and reduces venous return, causing blood pressure changes and reflex vasoconstriction. In both tests, the pattern of responses is an index of adrenergic function.
PROVEN CARE STANDARDS
Testing of the autonomic nervous system is recommended for early detection of diabetes and a standard of care by the American Diabetes Association for patients with Type 1 and Type 2 diabetes.

The American Heart Association Practice Guidelines for the management of patients with Peripheral artery disease include the measurement of ankle brachia I index (ABI) in adults 50+ years old with history of smoking diabetes, or circulation problems, and all adults above 70 years old.

NON-INVASIVE ACCURACY
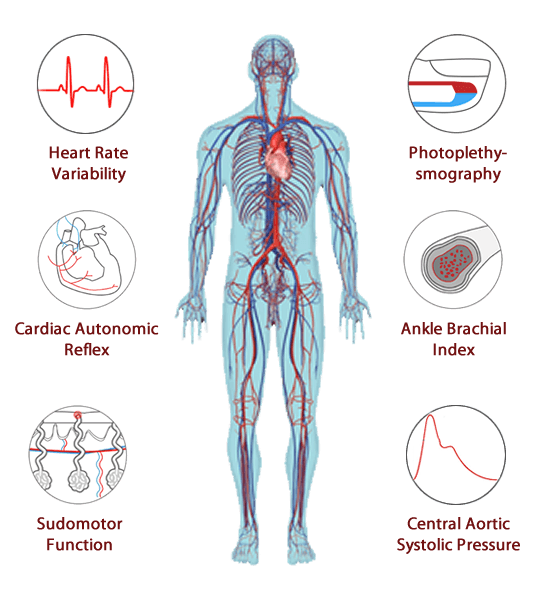
ANS state-of-the-art testing performs a series of non-invasive tests which aid in the identification and early detection of autonomic nervous system & arterial dysfunction related to disorders and disease complications.
- Quantitative assessments of the autonomic nervous system (ANS)
- Distinguishes between early and late stages of autonomic neuropathy
- Test for cardiovascular autonomic neuropathy (CAN)
- Test for diabetic autonomic neuropathy (DAN) Diabetes Management
- Cardiovascular Assessment
How serious is autonomic dysfunction?
Autonomic dysfunction can range from mild to life-threatening. It can affect part of the ANS or the entire ANS. Sometimes the conditions that cause problems are temporary and reversable. Others are chronic, or long term and may continue to worsen over time.
Early detection and treatment are very important reducing or possible addressing the issue in the early stages.
What are the symptoms of autonomic dysfunction?
A key feature of autonomic dysfunction, either orthostatic syncope or presyncope, should guide us to suspicion of cardiovascular autonomic dysfunction. In this scenario, the usual symptoms are dizziness, giddiness, blurred or tunnel vision, headache, or neckache (coat-hanger pain), nausea, or fatigue.
What diseases cause autonomic dysfunction?
Autonomic nervous system disorders can occur alone or as the result of another disease, such as Parkinson's disease, cancer, autoimmune diseases, alcohol abuse, or diabetes.
How can we improve ANS?
Upon completion of ANS testing, your doctor has a report with all the data from the test. The doctor will use this information in an evaluation with you.
A second report for the patient gives information about risk factors found for you. This report provides information what you can do to improve your ANS.
ANS Testing Measures 8 Risk Factors
1. AUTONOMIC NERVOUS SYSTEM DYSFUNCTION RISK
Problems with the ANS can range from mild to life threatening. Sometimes only one part of the nervous system is affected. In other cases, the entire ANS is affected. Some conditions are temporary and can be reversed, while others are chronic and will continue to worsen over time. Diseases such as Diabetes or Parkinson’s disease can cause irregularities with the ANS. Problems with ANS regulation often involve organ failure, or the failure of the nerves to transmit a necessary signal.
2. SUDOMOTOR DYSFUNCTION RISK
Sudomotor dysfunction testing may indicate to physicians of a patient’s peripheral nerve and cardiac sympathetic dysfunction. Neuropathy is a common complication in diabetes mellitus (DM), with 60%–70% of patients affected over lifetime. Symptoms of neuropathy are very common, and subclinical neuropathy is more common than clinical neuropathy. Neuropathy may remain undetected, and progress over time leading to serious complications. The most common associated clinical condition is peripheral neuropathy, affecting the feet. Autonomic nerve involvement is common but probably the most undiagnosed. Low scores in the sudomotor may lead a medical provider to look at clinical neuropathy.
3. ENDOTHELIAL DYSFUNCTION RISK
Current evidence suggests that endothelial function is an integrative marker of the net effects of damage from traditional and emerging risk factors on the arterial wall and its intrinsic capacity for repair. Endothelial dysfunction, detected as the presence of reduced vasodilating response to endothelial stimuli, has been observed to be associated with major cardiovascular risk factors, such as aging, hyperhomocysteinemia, post menopause state, smoking, diabetes, hypercholesterolemia, and hypertension.
4. PLETHYSMOGRAPHY CARDIOVASCULAR DISEASE RISK
The PTG CVD risk factor is the combined total of the other seven risk factors assessments. It takes into consideration the cardiovascular, as well as, the autonomic nervous system (ANS) measurements.
5. SMALL FIBER NEUROPATHY RISK
A small fiber neuropathy occurs when damage to the peripheral nerves predominantly or entirely affects the small myelinated fibers or Unmyelinated C fibers. The specific fiber types involved in this process include both small somatic and autonomic fibers. The sensory functions of these fibers include thermal perception and nociception. These fibers are involved in many autonomic and enteric functions
6. INSULIN RESISTANCE RISK
Insulin resistance is defined clinically as the inability of a known quantity of exogenous or endogenous insulin to increase glucose uptake and utilization in an individual as much as it does in a normal population. Insulin resistance occurs as part of a cluster of cardiovascular‐ metabolic abnormalities commonly referred to as “The Insulin Resistance Syndrome” or “The Metabolic Syndrome”. This cluster of abnormalities may lead to the development of type 2 diabetes, accelerated atherosclerosis, hypertension or polycystic ovarian syndrome depending on the genetic background of the individual developing the insulin
7. CARDIOMETABOLIC RISK
The specific factors that can cause this increased risk include: obesity (particularly central), hyperglycemia, hypertension, insulin resistance and dyslipoproteinemia. When patients have one or more risk factors and are physically inactive or smoke, the cardiometabolic risk is increased even more. Medical conditions that often share the above characteristics, such as type 2 diabetes, can also increase cardiometabolic risk. The primary focus of cardiometabolic risk treatment is management of each high‐risk factor, including dyslipoproteinemia, hypertension, and diabetes. The management of these subjects is based principally on lifestyle measures, but various antihypertensive, lipid‐lowering, insulin sensitizing, anti‐obesity and antiplatelet drugs could be helpful in reducing
8. CARDIAC AUTONOMIC NEUROPATHY RISK
High blood glucose levels over a period of years may cause a condition called autonomic neuropathy. This is damage to the nerves that control the regulation of involuntary function. When the nerve damage affects the heart, it is called cardiac autonomic neuropathy (CAN). CAN encompasses damage to the autonomic nerve fibers that innervate the heart and blood vessels, resulting in abnormalities in heart rate control, vascular dynamics and the body’s ability to adjust blood pressure. CAN is a significant cause of morbidity and mortality associated with a high risk of cardiac arrhythmias and sudden death.
The testing equipment

TM Flow Patient Test (General Practice) 2018 Gateway Clinical
Patient being tested with TM Flow Autonomic Nervous System and Vascular Function Assessment by LD Technology.